MEDICAID REDETERMINATION
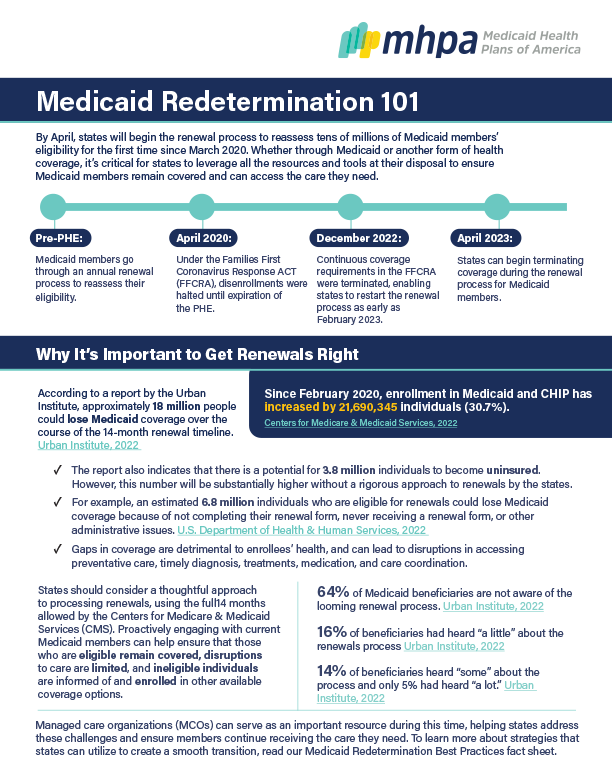
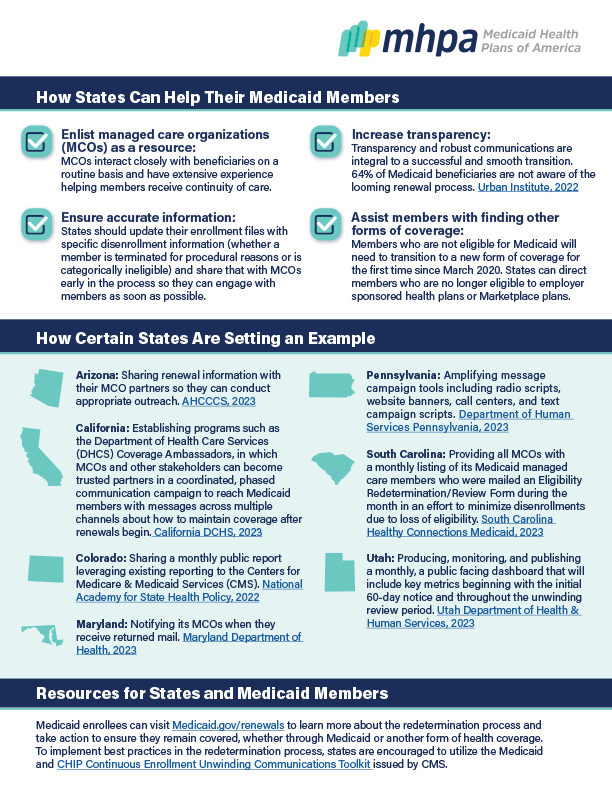
After a three-year period in which Medicaid beneficiaries were not disenrolled, states must resume the process of redetermining eligibility. Watch MHPA President and CEO Craig Kennedy, MPH, explain why it's imperative to get renewals right and how managed care organizations (MCOs) are partnering with states to ensure that eligible individuals maintain Medicaid coverage, and those who no longer qualify for Medicaid have access to other coverage in the Marketplace.
Reports indicate that 18 million people could lose coverage during the redetermination process. And an alarming 64% of Medicaid beneficiaries are unaware that it's taking place. The resources below capture the scope of Medicaid redetermination, detrimental effects of coverage loss, and best practices that states can employ for a smooth transition.
For further inquiries or more information, please contact us directly at:
Shannon Attanasio, Government Relations & Advocacy, sattanasio@mhpa.org
Jeanine Boyle, Policy, jboyle@mhpa.org