Research & Reports
MHPA’s research demonstrates the state and value of Medicaid managed care to help inform policy, deepen understanding of performance, and drive quality.
.October 2024 -
The Waiver Effect:
An Exploratory Analysis of Medicaid Enrollment Trends in the Presence of Waivers
New research from MHPA reveals that Medicaid Managed Care Organization (MCO)-specific waivers significantly impact enrollment during the unwinding of continuous enrollment. Our analysis of a full year of data shows that states utilizing two waivers experienced the lowest decline in net Medicaid enrollment (11.9% loss) compared to states with zero waivers (15.8% loss).
VIEW THE RESEARCH BRIEF
July 2024 -
 Snapshot of Medicaid with Managed Care - UPDATED
Snapshot of Medicaid with Managed Care - UPDATED
Medicaid managed care organizations (MCOs) partner with states to improve access to primary, preventive, and specialty services for the nation’s most vulnerable populations. The managed care model provides flexibility to address the local, diverse, and complex needs of Medicaid enrollees and improve health outcomes.
As state Medicaid agencies complete post-pandemic eligibility requirements, MCOs continue to play an important role in meeting the health care needs of Medicaid enrollees.
VIEW THE INFOGRAPHIC
January 2024 -
 State of Medicaid Managed Care: A Closer Look at Managed Long-Term Services and Supports
State of Medicaid Managed Care: A Closer Look at Managed Long-Term Services and Supports
To better understand Managed Long-Term Services and Supports (MLTSS) programs, which vary widely in the populations and benefits included under managed care, Sellers Dorsey partnered with MHPA, the Association for Community Affiliated Plans (ACAP), and the National MLTSS Health Plan Association to release "The State of Medicaid Managed Care: A Closer Look at MLTSS." The report features a:
-
Breakdown of key program features of states at various points in the development of MLTSS programs.
-
Survey of states currently operating an MLTSS program on program priorities, dual eligible integration, and more.
-
In-depth look at states' experiences with MLTSS programs including the PHE, Dual Eligibles, Workforce Challenges, and more.


 On the Ground Enrollment: Results from a National Survey of Medicaid MCO Experiences During Redetermination
On the Ground Enrollment: Results from a National Survey of Medicaid MCO Experiences During Redetermination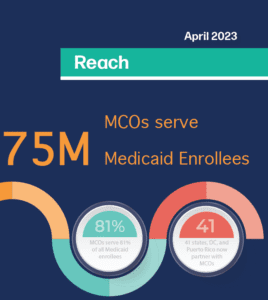 April 2023 -
April 2023 -